In this article, we delve into six specific malocclusion conditions with the strongest link to TMJ pain and TMD, highlighting the connection between dental alignment and jaw joint orthopedics and function. By understanding these correlations, individuals can grasp the importance of addressing malocclusion early to prevent imbalances that could contribute to TMJ-related issues, fostering better oral health and overall well-being.
What is Malocclusion?
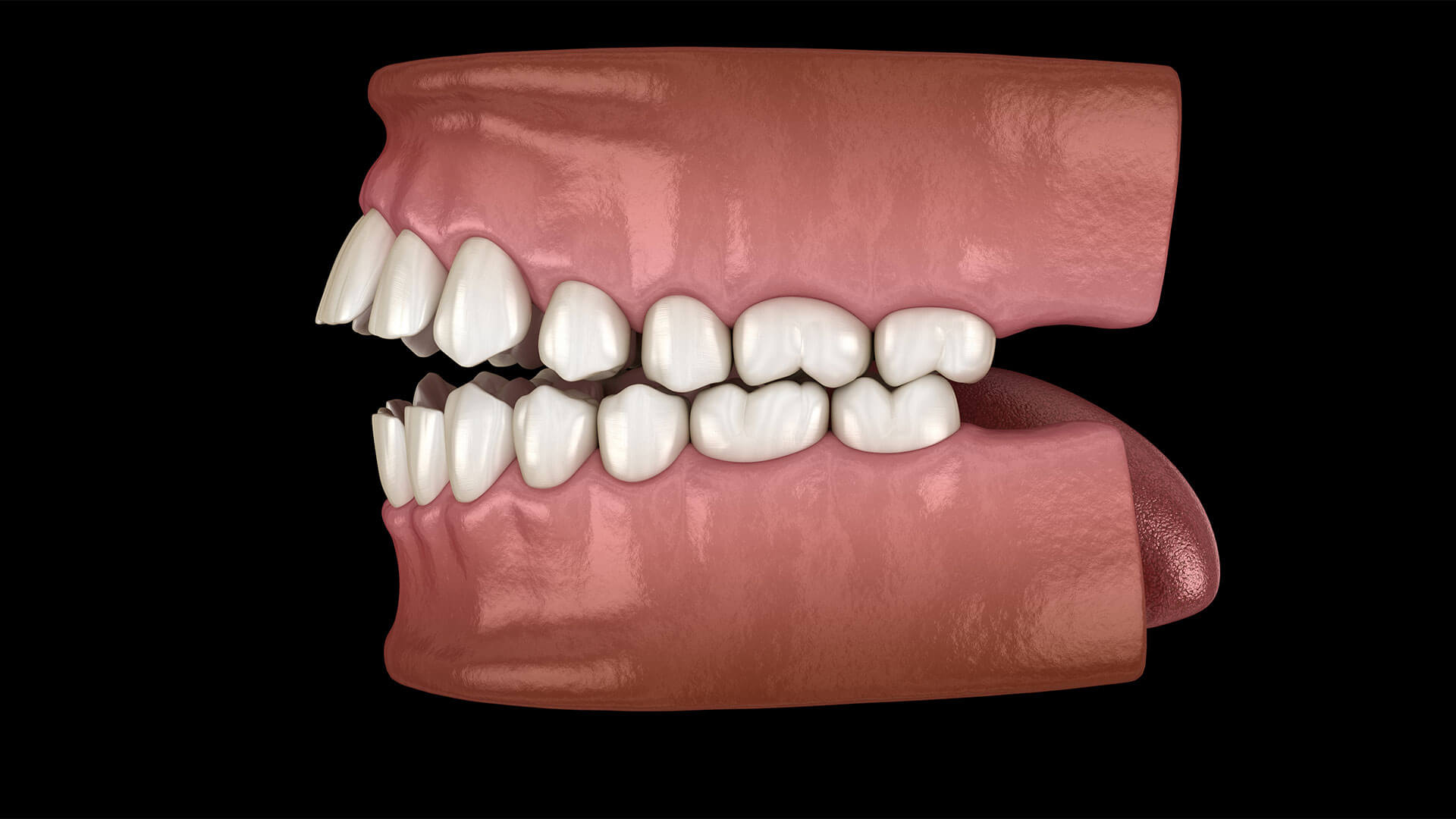
Malocclusion refers to the misalignment or incorrect positioning of the teeth when the jaws are closed. This misalignment can occur in various forms, such as crowded teeth, crooked teeth, overbites, underbites, crossbites, and open bites. Malocclusion can affect both the aesthetics of the smile and the function of the bite, leading to difficulties with chewing, speaking, and maintaining oral hygiene. It can also contribute to various dental issues, including tooth wear, gum disease, and temporomandibular disorders (TMD). Treatment for malocclusion may involve orthodontic intervention, such as braces or aligners, to correct the alignment of the teeth and jaws and improve overall oral health and function.
What is TMJ Pain and TMD?
TMJ pain specifically refers to discomfort or pain in the temporomandibular joint (TMJ) itself. It may manifest as aching, tenderness, or soreness in the jaw joint or ear area. It can occur due to various factors, including injury, arthritis, or excessive strain on the joint.
TMD (Temporomandibular Disorders), on the other hand, is a broader term that encompasses a range of conditions affecting the temporomandibular joint (TMJ) and the surrounding muscles. It includes not only pain in the TMJ but also other symptoms such as difficulty chewing, clicking or popping sounds in the jaw joint, jaw locking, and muscle stiffness. TMD can result from various factors, including malocclusion, jaw injury, teeth grinding (bruxism), stress, or arthritis.
Specific Malocclusion Conditions Associated wiacth TMJ Pain and TMD
Traumatic Impinging of Deep Bite
This is a condition where the lower front teeth excessively bite into the gum tissue behind the upper front teeth due to an overbite or deep bite. This can cause trauma to the gum tissue, leading to irritation, inflammation, and potential complications such as gum recession and tooth mobility. It’s a situation where the misalignment of the teeth causes ongoing damage and discomfort in the mouth.
This condition can contribute to TMD and TMJ pain in several ways. In most cases, this condition is associated with a reduced lower facial height and a habit of severe clinching. Therefore, the constant pressure and trauma on the gum tissue can lead to inflammation and irritation. Over time, this can result in muscle soreness, jaw pain, discomfort, and dysfunction characteristics of TMD. Additionally, the misalignment caused by a deep bite can disrupt the normal function of the jaw joint, potentially exacerbating TMD symptoms. Therefore, addressing traumatic impinging of deep bite through orthodontic intervention and addressing the parafunctional habits may help alleviate TMD symptoms by reducing pressure on the gum tissue and restoring proper bite alignment.
Loss of Posterior Occlusion
Loss of Posterior Occlusion, a condition characterized by the absence of proper contact between the upper and lower back teeth (molars and premolars) when the jaws are closed, is a significant contributor to the development of TMJ pain and TMD. This malocclusion disrupts the natural distribution of bite forces due to the lack of posterior loading affecting the function of the jaw, leading to additional load and strain on the jaw muscles and joints. The resulting imbalance in association with a parafunctional habit of clinching and grinding could cause muscle tension, fatigue, and discomfort, ultimately manifesting as TMJ pain and TMD symptoms. Loss of Posterior Occlusion highlights the intricate relationship between malocclusion and TMJ-related issues, underscoring the importance of addressing bite irregularities to alleviate TMJ pain and improve overall oral health. Understanding and addressing this condition is crucial for both patients and practitioners in effectively managing TMJ-related concerns and enhancing quality of life.
Poor Dental Articulation
Dental articulation, the precise alignment and interaction of the teeth when the jaws come together, plays a crucial role in oral function and overall dental health. When dental articulation is compromised due to malocclusion, or improper alignment of the teeth, with the presence of a parafunctional habit it can contribute to the development of TMJ pain and TMD. Malocclusion disrupts the harmonious relationship between the upper and lower teeth, leading to uneven distribution of forces on the jaw joints and muscles. This imbalance can result in increased muscle tension, jaw discomfort, and ultimately TMJ pain and TMD symptoms. Understanding the significance of dental articulation in the context of malocclusion sheds light on its role as a contributing factor to TMJ-related issues, further emphasizing the importance of addressing bite irregularities to alleviate TMJ pain and improve overall oral health.
Anterior Open Bite
Anterior open bite, a common form of malocclusion, occurs when the front teeth of the upper and lower jaws do not make contact when the mouth is closed. This condition creates an opening or gap between the upper and lower front teeth, affecting both the aesthetics and function of the bite. An anterior open bite can lead to various complications, including difficulty chewing, speech problems, and increased risk of dental issues such as tooth wear and gum problems. Additionally, anterior open bite has been associated with TMJ pain and TMD. The imbalance in the bite and the body’s reaction to clinch to try to get the anterior dentition to occlude yet an anterior open bite is sustained. This cycle can result in strain on the jaw joints and muscles, contributing to TMJ pain and exacerbating TMD symptoms.
Functional Shift Caused by Unilateral Posterior Crossbite
Unilateral posterior crossbite with a functional shift is a specific form of malocclusion characterized by the misalignment of the upper and lower teeth on one side of the mouth. In this condition, the upper teeth do not properly align with the lower teeth when the jaws come together, leading to an asymmetrical bite pattern. This discrepancy can result in a functional shift, where the lower jaw shifts to one side during biting and chewing to compensate for the misalignment and try to make the teeth somewhat occlude. Unilateral posterior crossbite with a functional shift not only affects the aesthetics of the smile but also impacts the function of the jaw. The imbalanced distribution of orthopedic forces on the teeth and jaw joints can contribute to TMJ pain and TMD. By addressing unilateral posterior crossbite with a functional shift, individuals can alleviate TMJ pain and improve overall oral health and function.
Anterior Crossbite
Anterior crossbite is a type of malocclusion characterized by the misalignment of the upper front teeth with the lower front teeth when the jaws are closed. This is different from an underbite, which happens when all your top teeth are behind your bottom teeth. In this condition, the upper front teeth sit behind the lower front teeth, creating an abnormal bite relationship. Anterior crossbite not only affects the aesthetics of the smile but also impacts the function of the jaw. Like many other malocclusions, the misalignment can lead to uneven wear of the teeth, difficulty biting and chewing, and even speech problems. Additionally, the imbalance in the bite caused by anterior crossbite can result in strain on the jaw joints and muscles, which may contribute to TMJ pain and exacerbate TMD symptoms.

Malocclusion Treatment
As we wrap up our discussion on studying the connections between malocclusion, TMJ pain, and TMD, Dr. Daia urges clinicians to embrace a new approach in TMD practice. Abandoning the old gnathological paradigm, he advocates for an interdisciplinary, comprehensive approach that addresses the neuromuscular and orthopedic complexities while achieving functional occlusion. With this holistic perspective, specialists can provide their patients with the highest level of care. If you’re experiencing any symptoms of TMJ pain or suspect malocclusion may be a contributing factor, we invite you to schedule a free consultation with us. Together, we can embark on a journey towards improved oral health and overall well-being. Don’t wait any longer – book your evaluation today and take the first step towards a brighter, pain-free future.




